-
-
The elderly and diabetes: everything you need to know
Carolyn contacted The Diabetes Council…
When Carolyn contacted TheDiabetesCouncil, she was concerned about her mother who is elderly and is living with diabetes. She didn’t know much about her medications, or how they might interact with her other medications. She was worried that her mother’s low blood sugar while she was home alone may be related to her worsening memory.
Science call this the most dangerous ingredient for body fat…
In the following article we will explore many different guidelines and recommendations, along with nutritional, activity, pharmaceutical, and financial and estate planning considerations. Those are just a few of the issues that we will touch on related to the elderly with diabetes. So let’s get started with some general and medication considerations first…
General guidelines for the elderly with diabetes
The following are some general guidelines to consider when treating the elderly with diabetes:
Medication considerations for the elderly with diabetes
The elderly population has a decreased ability to metabolize medications in some cases. Associated electrolyte imbalances, and increased effects of adverse symptoms with polypharmacy make managing medications for diabetes in the elderly especially challenging. The following are some medication considerations for the elderly with diabetes:
The diabetes care team for an elderly patient with diabetes should consist of certified diabetes educators, nurses, doctors or other primary care providers, nutritionists, physical therapists, pharmacists, and others who will appropriately plan and coordinate care for the elderly patient with diabetes.2
American Association of Diabetes Educators senior guide
The ADA developed a guide for adults age 55 and older with diabetes. It includes basic information about diabetes, how to eat healthy, get enough exercise, take medications for diabetes, and what to expect at doctor visits when you have diabetes. You can also find information on travelling, complications, paying for healthcare, and information for caregivers. You can read more about it here: http://main.diabetes.org/dorg/PDFs/living-with-diabetes/living-healthy-with-diabetes-guide.pdf
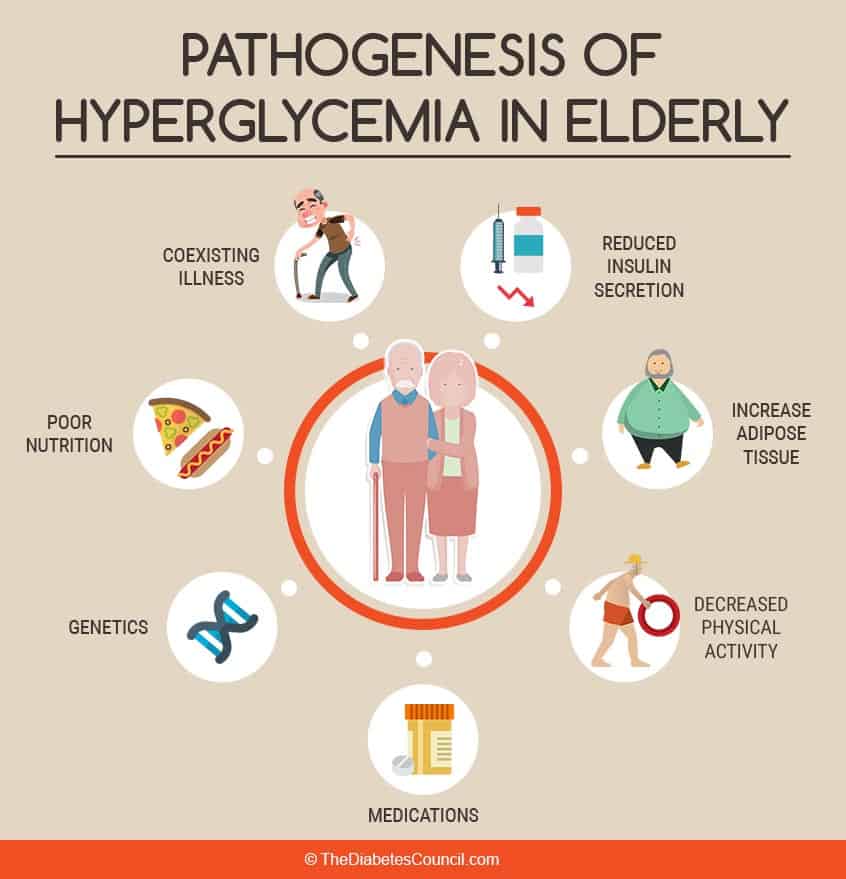
Diagnosis of diabetes in the elderly is not so straight forward
Sometimes the diagnosis of diabetes in the elderly can be a bit tricky. They may be displaying symptoms of confusion and urinary incontinence, dry mouth, or other vague signs, and not showing all of the usual symptoms of diabetes. They may become dehydrated, and have electrolyte imbalances. This is due, in part, to how the kidneys metabolize blood sugar in the elderly.
Health factors that increase problems in the elderly with diabetes
High blood pressure, high LDL cholesterol and triglycerides, decreased mentation, symptoms and feelings of depression, and decline in ability to perform activities of daily living are all health factors that cause problems for the elderly with diabetes. In a study of seniors with diabetes, a full one-third of patients over age 70 showed signs of dementia that was correlated with high blood sugars.
It is shown that the elderly with diabetes die younger, and have more falls related to low blood sugars that cause a decrease in mobility and lead to a decline in the quality of life for this population. They are more likely to utilize assistive aids, such as canes, walkers, bedside commodes, and the like.
The elderly with diabetes are at an even greater risk of forgetting to eat regular meals and snacks, being unable to afford food that fits into their diabetes plan, or unable to cook their own meals at home. They are at greater risk of being unable to afford their medications.
Glycemic targets for the elderly with diabetes
Glycemic targets of A1C and blood sugar levels can be relaxed for those seniors with diabetes, especially if there are underlying health factors such as cardiovascular disease or episodes of low blood sugars.
Case Study:
I had an elderly gentleman with diabetes and cardiovascular disease come in for diabetes education. He was 83 years old at the time. His A1C was 7.4, but he was having low blood sugars, generally about 2-3 per week. Knowing that this was a safety risk factor for this gentleman, his physician was contacted, and his A1C target was relaxed to 8.0. He worked with the dietitian to adjust his diet to prevent further episodes of low blood sugars.
An elderly person with diabetes who is in great shape, and otherwise has no other health problems, functional or activity impairments, or cognitive impairments may be fine with an A1C of 7.0 to 7.5 percent. However, if there are other underlying health issues, functional and activity limitations, or cognitive impairments, A1C targets should be relaxed. A 7.6 to 8.5 percent A1C value may be better suited for those who are having frequent episodes of hypoglycemia, or who have the aforementioned health issues.
The goal is always to prevent low blood sugars when working with the elderly with diabetes, while balancing a need to avoid acute problems of high blood sugars and complications of diabetes. Hypoglycemia unawareness is more common in the elderly due to decreased counter-regulatory mechanisms. Avoiding falls related to low blood sugar is important for the elderly with diabetes, as falls lead to increased morbidity.
The elderly with diabetes and nutrition

Elderly patients with diabetes should be encouraged and assisted in obtaining the appropriate nutrition. Regular meals and snacks are needed for this population as with others, but with increased risk of low blood sugars, this becomes even more important in seniors.
Set reminders, give reminders:
Setting alarms, or having caregivers remind them when it is time to take their medications and eat their meals or snacks, along with setting up a medication dispenser to help with medication compliance, helps seniors with diabetes manage their diabetes appropriately. They should wear proper identification bracelets that identify them as a person with diabetes, and be encouraged to carry quick-acting carbohydrates with them at all times for when they may have a low blood sugar. Glucose tablets, glucose gel, or juice boxes should be carried at all times to prevent a low blood sugar.
Diet and nutrition still can help manage when you are a senior adult with diabetes
You can still go far in managing your diabetes by incorporating an appropriate diet and moderate exercise into your routine as an elderly person with diabetes. In “Treating the elderly diabetic patient: special considerations”, Kezerle et all give the following recommendation to elderly patients with diabetes : Although most patients with DM2 will require medication over the course of their disease, there is enough evidence to support the fact that older persons can respond well to nutrition therapy and exercise.

The elderly with diabetes and exercise
Exercise should be tailored to fit each individual senior with diabetes and must take into account any health conditions that might affect the ability to exercise. Working with an exercise physiotherapist, or a physical therapist, may be needed. At any rate, a senior with diabetes should discuss what would be an appropriate exercise program for their diabetes that takes into account all limitations, and keeps them safe while exercising.
Senior centers offer a variety of programs including “Geri-Fit,” “Tai Chi,” varied yoga classes for seniors, and walking groups, as well as many other exercise programs that improve balance and coordination and decrease insulin resistance in the elderly with diabetes.
Some seniors with diabetes may be able to participate in all kinds of exercise classes and activities, while others may need a chair exercise program, or something in between related to their personal fitness level.
Teaching tools for the elderly with diabetes
Instruction by diabetes educators should be provided, presenting one concept at a time, making sure that the patient can hear instructions. Write instructions down in large print, and provide aids such as a magnaguide for drawing up of insulin doses. Decide between teaching carbohydrate counting and a food group planning curriculum, as some older adults may prefer the later.
Refer to appropriate community resources:
The elderly with diabetes should be referred to the appropriate community resources in their communities, including the Area Agency on Aging, local senior centers , diabetes support groups, exercise and walking groups, meals-on-wheels, or other social services.3
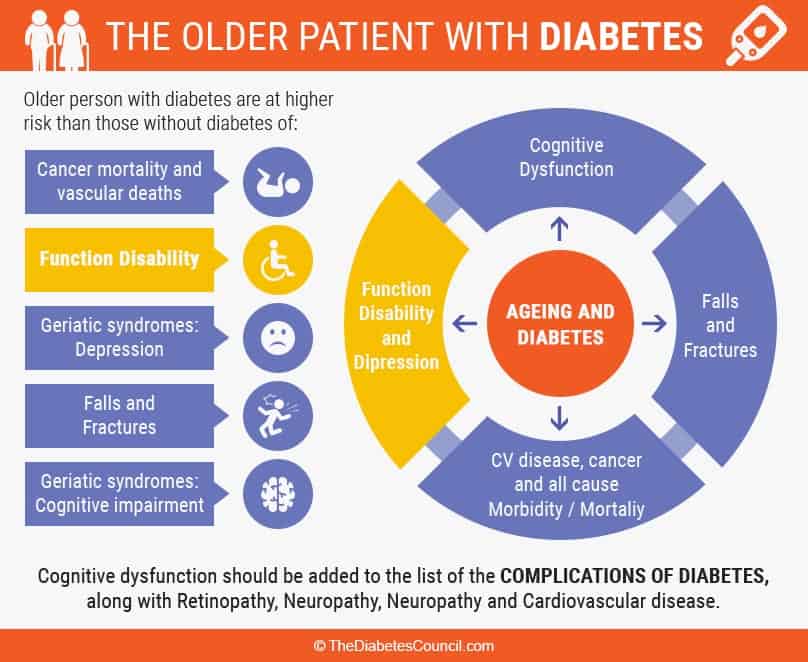
Elderly with diabetes are at a greater risk for diabetes complications
The older population with diabetes is at a greater risk of developing the complications of diabetes than their younger peers with diabetes. As a senior, even if you are good at self-managing your diabetes, you are still at an increased risk of developing hearing and vision problems, developing memory loss and other cognitive impairments, and/or mobility difficulties that effect activities of daily living.
Conversely, these complications are increased in the elderly whose diabetes isn’t very well managed. As we shall see, the culprit is almost always high blood sugar; therefore managing blood sugars over the long haul will help to avoid these complications. The main complications of diabetes that especially effect the aging population are:
1) Problems with hearing
Although hearing problems are common in older adults, an elderly person with diabetes is two times as likely to have a marked hearing loss. Although there is currently no cure for hearing loss, hearing aids provide an appropriate assistive technology. They are costly though, with some models costing about $6-7000.
2) Problems with vision
Vision can be a double-whammy for the person with diabetes. Though they have all of the usual problems with vision as a result of aging in general, they also have the constriction of blood vessels that causes destruction of eye vessels that comes with diabetes. On top of that, they may have high blood pressure also, which further compromises vision and eye health. Diabetic retinopathy, which can now be treated in many cases with lasers, will repair the damage, but overall long-term blood sugar management is needed to prevent reoccurrence.
3) Problems with memory and cognition
Diabetes affects the brain of the elderly by depositing plaques in the brain, which impede impulse transmission and cause problems with memory and cognition. In addition, mood problems may become worse as people with diabetes age.
It’s a “Catch 22,” because to manage your diabetes, you need to have full function of your cognitive capacities. Therefore, one problem may precipitate another. Careful screening is needed, and the elderly with diabetes may need assistance from outside services, or a care giver.
4) Problems with joints and bones
As we age, our joints become worn and tender, and it may become rather difficult for us to get around as we used to. Persons with diabetes are no different, but the disease also precipitates worsening symptoms of arthritis and other joint diseases. Nerve damage, called neuropathy, is common in the elderly with diabetes, and they have increases pins and needles and burning sensations in their extremities. Again, careful self-management reduces these symptoms of nerve damage in the older population with diabetes.4
So what can you do if you are elderly, and you have been diagnosed with diabetes?

It’s no fun to get the diagnosis of diabetes when you are already getting older, and have other health issues and concerns already. Your health care provider may prescribe a combination of diet, exercise, and medications to help you manage your new diagnosis of diabetes. Your health care team should look at all of your health issues, and help tailor a plan that is individualized for you. You should see a certified diabetes educator (CDE) to learn about all the aspects of self-management that you will need to know in order to decrease your risks for the complications of diabetes.
You will need to learn to self-manage your diabetes by:
Keeping a blood sugar log, tracking your blood sugars via the memory on your meter, or through an app on your smart phone: Talk with your doctor about getting your own home blood glucose meter, and meet with a CDE to learn how to operate your meter and track your blood sugar levels, and use your results to better manage your diabetes
Learning to read labels, learning appropriate portion sizes, learning how different foods affect your blood sugar, and learning which foods are appropriate choices for diabetes, and which foods you should leave for a special occasion or treat: Get help with meal planning from a nutritionist, and learn how to grocery shop, eat more lean meats, whole foods such as fruits and vegetables, and whole grains, and how to incorporate good fats into your diet, among many other things
Planning an activity program: Learn how exercising effects blood sugar and insulin levels, and work with your diabetes care team to develop an exercise and activity program to meet your personal and healthcare needs
In addition, keep the following regular appointments for your diabetes care:
Planning for elder years
We are all living longer, so it stands to reason that we need to plan for our elder years. It’s no fun to think about dying, which is probably why many people put off planning for the future. However, it protects you and those you leave behind if you do some careful planning related to your healthcare, long term care, and end of life planning.
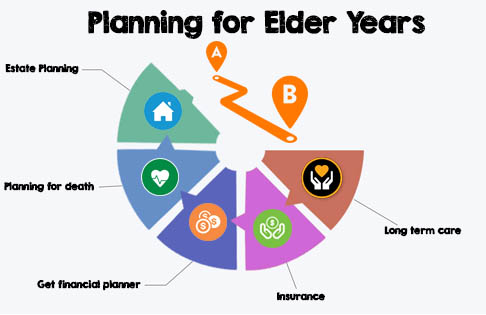
Long term care:
Planning will include looking into long term care options. As we age, we may have difficulty performing daily life activities such as getting dressed in the morning, cleaning our house, or cooking our meals. We may have trouble giving ourselves a bath, or even getting in and out of the tub or shower.
At the point when we are no longer able to do the things that we used to do for ourselves, we will need to think about whether we can stay at home. It’s possible that we may be able to get assistance in our own home. If we are having more severe issues with diabetes, we may need to look at moving into an assisted living facility, or even a nursing home.
You will want to make sure that you make plans that outline who you want to make decisions for you in the event that you are unable to make important decisions for yourself.
Long term care insurance:
Generally, your insurance policy will not cover the cost of long term care, whether in your home or in an assisted living facility or nursing home. Although Medicare may cover some of long term care costs, it doesn’t cover all of them. For Medicaid to cover it, you have to spend down money from savings for long term care to be covered.
Get a certified financial planner:
A certified financial planner can help you plan for the future, along with purchasing long term care insurance. You should contact your local Area Agency on Aging. You can get all kinds of advice related to home health, legal help, nursing services available, and assistance with delivery of meals (Meals-On-Wheels).
Planning for death:
Everyone needs to plan for death, regardless of how unpleasant the idea may seem. If you want to make sure that the things that you have go to the people in your life that you want them to go to, then you have to have a plan. You may want to have a written plan that lets loved ones know if you prefer cremation over burial. You will want to adopt a Living Will, and Power of Attorney.
This outlines what kind of life support you want to be on if you were to lose the ability to breathe on your own, and who will have the authority to “pull the plug,” and handle your affairs in this unfortunate situation.
You will want to list all of your financial accounts, including access information. This would include safe deposit boxes, insurance policies and other important personal papers, and key persons to contact. People to contact may include estate planning lawyers, funeral directors, and the like.
Estate Planning:
Estate planning includes provisions of a last will and testament. It should include a letter that is based on your intent in the event that you are unable to make your wishes known. You could even plan your entire funeral, right down to flowers and the casket, the music and the food. Perhaps you would rather have your relatives have a party, and celebrate your life, instead of dwelling on the details of planning your funeral. Lawyers to assist with estate planning are available in most communities, as are funeral directors.6
End of life (palliative care and hospice)
Low blood sugar prevention is the #1 priority
The one thing of the utmost importance with the elderly with diabetes and palliative care is the prevention of low blood sugar. It’s complicated, because the elderly with diabetes in long term care facilities are great in numbers, due to the increased prevalence of diabetes as we age. Treatments that are individualized are needed, even with the increased prevalence. This should be paramount, and contributes to the increased cost of palliative care in the elderly with diabetes.
Set targets higher
Blood sugar and A1C targets should be individualized to prevent low blood sugars that contribute to morbidity in this population. The American Diabetes Association developed a position statement that breaks down this population in long term care facilities. There is a need to look at all of the diagnoses that may be affecting an individual with diabetes in a long term facility, and to avoid the use of system-wide sliding scale coverage.
ADA Position Statement on End of Life, palliative and hospice care for the elderly with diabetes
Points of note in the ADA position statement are to take a close look at the blood sugar lowering medications that are used, and also to replace Social Security Income (SSI) in long term facilities. One thing that puts patients with diabetes in these facilities at greater risk is the high turnover in nursing homes, and the likelihood of being shuffled around. Patients may see multiple doctors and providers, with no one really knowing their individual needs related to their diabetes, thus increasing the risk of low blood sugar.
The ADA position further stresses the need for increased diabetes management, and a multidisciplinary team to treat the patient in palliative or hospice care, sometimes referred to as end of life care. The ultimate goal for end of life care is to prevent low blood sugar and increasing the patient with diabetes’ quality of life.
Aging, and increased prevalence of diabetes
Diabetes is indeed an epidemic, and as we continue to live longer, we will have more diabetes. As we age, our risk of developing diabetes is a full six times that of a person in their 20s. It is even higher in nursing homes, and hospice care facilities, and tops out at a whopping 34 percent.
Higher health costs for diabetics in long term facilities
That translates to higher health care costs, as the elderly in palliative care with diabetes have more than double the cost of others their age in long term care without diabetes. The total cost was estimated at over 19 billion in 2012.